TUBULAR EXTERNAL FIXATORS
- Home Page
- TUBULAR EXTERNAL FIXATORS
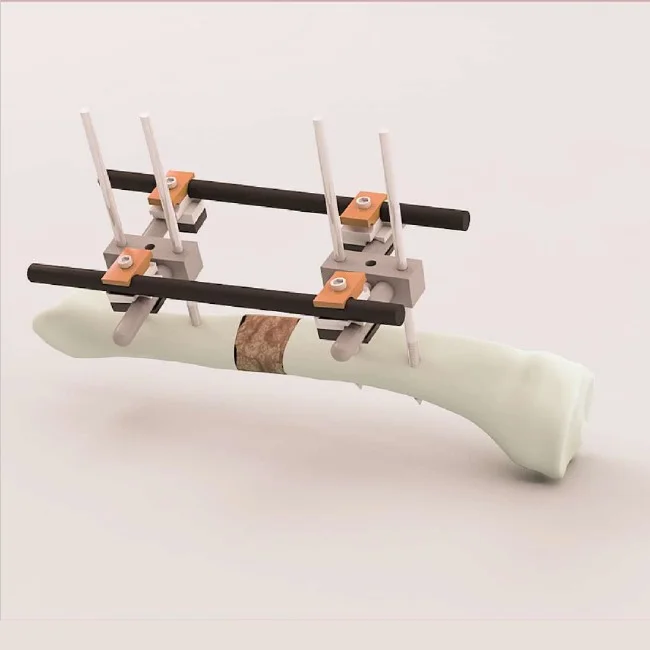
Tubular External Fixator: Components and Clinical Applications
Introduction
The tubular external fixator represents a versatile and modular system for fracture stabilization and deformity correction in orthopedic trauma surgery. First introduced in the 1970s, this system has evolved into a cornerstone of contemporary orthopedic practice, particularly in the management of complex fractures, osteotomies, and limb reconstruction scenarios (Müller et al., 1979). The system's adaptability to various anatomical regions and its capacity for gradual adjustment make it particularly valuable in both acute trauma and elective reconstructive settings.
Components of the Tubular External Fixator System
The tubular external fixator system comprises several key components that can be configured in multiple ways to address specific clinical requirements:
1. Structural Elements
- Tubular rods: Typically 10-11mm in diameter, available in various lengths (150-500mm). Constructed from stainless steel or titanium alloys for optimal strength-to-weight ratio.
- Connecting clamps: Universal clamps that permit multi-planar fixation between rods and pins/wires. Most modern systems allow 360° rotation with secure locking mechanisms.
- Articulations: Ball joints and swivel clamps that enable complex three-dimensional configurations when needed.
2. Bone Interface Components
- Schanz screws: Partially threaded pins (4-6mm diameter) with self-drilling or self-tapping tips. Available in various lengths (50-250mm) and thread designs.
- Transfixion wires: 1.5-2.0mm diameter smooth or olive wires for hybrid fixation, particularly in metaphyseal regions.
- Wire fixation bolts: Specialized clamps for secure fixation of tensioned wires to the frame.
3. Supplementary Components
- Dynamization devices: Allow controlled axial loading of fractures during healing.
- Reduction instruments: Specialized clamps and distractors for intraoperative fracture reduction.
- Pin-to-rod connectors: Enable connection of pins directly to rods without intervening clamps in certain configurations.
Clinical Applications
The versatility of tubular external fixation makes it applicable across a broad spectrum of orthopedic conditions:
1. Trauma Indications
| Fracture Type | Configuration | Considerations |
|---|---|---|
| Open fractures (Gustilo III) | Unilateral or bilateral frame | Allows wound access, can be converted to internal fixation later |
| Comminuted periarticular fractures | Hybrid fixation (wires + pins) | Preserves metaphyseal blood supply, minimal soft tissue disruption |
| Pelvic ring disruptions | Anterior or circumferential frame | Emergency stabilization in hemodynamically unstable patients |
| Severe upper extremity trauma | Miniaturized components | Small-diameter pins (3-4mm) to avoid neurovascular structures |
2. Reconstructive Applications
- Limb lengthening: Gradual distraction via daily adjustments (Ilizarov technique)
- Deformity correction: Multiplanar correction of angular, rotational, and translational deformities
- Infected nonunions: Stable fixation while permitting debridement and antibiotic treatment
- Arthrodesis: Temporary stabilization during joint fusion procedures
Biomechanical Principles
The effectiveness of tubular external fixation relies on several biomechanical principles:
- Frame stiffness: Determined by pin diameter, number of fixation points, and frame configuration. Stiffness increases with:
- Larger pin diameter (exponential relationship)
- Increased pin spread (distance between proximal and distal pin clusters)
- Additional connecting rods (double-stack configurations)
- Pin-bone interface: The weakest link in the system. Heat generation during pin insertion should be minimized to prevent thermal necrosis.
- Fracture biology: Appropriate dynamization at later stages promotes callus formation while maintaining alignment.
Operative Technique Highlights
1. Preoperative Planning
- Determine safe corridors for pin placement based on cross-sectional anatomy
- Select appropriate pin diameter (generally ≤1/3 of bone diameter)
- Plan frame configuration based on fracture pattern and required stability
2. Surgical Application
- Reduce major fracture fragments (closed or limited open)
- Insert Schanz screws through stab incisions using soft tissue protection sleeves
- Assemble connecting rods approximately 2-3cm from skin to allow for swelling
- Apply final tightening after confirming alignment clinically and radiographically
3. Postoperative Management
- Daily pin site care with saline or dilute antiseptic solutions
- Early mobilization when fracture stability permits
- Regular radiographic monitoring of fracture alignment and healing
- Gradual dynamization in appropriate fracture patterns
Complications and Mitigation Strategies
| Complication | Incidence | Preventive Measures |
|---|---|---|
| Pin site infection | 15-30% | Proper insertion technique, regular pin care, early antibiotic treatment |
| Pin loosening | 10-20% | Avoid thermal necrosis during insertion, appropriate pin diameter |
| Neurovascular injury | <5% | Thorough knowledge of safe corridors, blunt dissection to bone |
| Malunion | 5-15% | Intraoperative imaging, proper frame configuration, follow-up adjustments |
Recent Advances
Modern developments in tubular external fixation include:
- Carbon fiber rods: Radiolucent material permits improved radiographic visualization
- Computer-assisted correction: Software-guided gradual deformity correction
- Antimicrobial coatings: Silver or antibiotic-impregnated pins to reduce infection risk
- Hybrid fixation systems: Integration with internal fixation techniques
Conclusion
The tubular external fixator remains an indispensable tool in the orthopedic surgeon's armamentarium, offering unparalleled versatility in both trauma and reconstructive scenarios. When applied with attention to biomechanical principles and proper surgical technique, it provides effective stabilization while minimizing additional trauma to compromised soft tissue envelopes. Continued technological advancements promise to further enhance the utility and reduce the complications associated with this time-tested fixation method.
References
- Müller ME, Allgöwer M, Schneider R, Willenegger H. Manual of Internal Fixation. Springer-Verlag; 1979.
- Fragomen AT, Rozbruch SR. The mechanics of external fixation. HSS J. 2007;3(1):13-29.
- Behrens F. General theory and principles of external fixation. Clin Orthop Relat Res. 1989;(241):15-23.
- Paley D. Principles of Deformity Correction. Springer; 2002.
- Egol KA, Nauth A, Lee M, et al. Bone healing in fracture treatment. Injury. 2017;48 Suppl 1:S1-S3.
